We often ascribe human traits to objects that do not have thoughts
or feelings of their own. This is called anthropomorphism,
and it is hard to go through a day without committing this faux pas.
I can think of one case in particular where individual cells of a
multicellular organism seem to be acting with a purpose, even a sense of
altruism. It is called apoptosis or programmed cell death. In apoptosis (from
Greek meaning, “falling off”) a cell will die “in order to” contribute to the
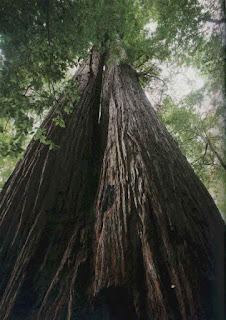
overall health of the organism. It happens all the time. Autumn is full of
apoptosis, as this is the mechanism of leaves falling, and is where the
original word came from.
You just had about 1 million of your cells die as a result of
apoptosis! … There! It just happened again! About a million cells/sec “commit
suicide” (there’s some more anthropomorphism) so that you can live. If they
didn’t die, you would.
It starts early, when you were in your embryonic stage. Your hands
and feet started as single masses, with the bones growing in the appropriate
places, at 48 days the skin covering is them all was one unit, more of a
mitten than a glove.
In terms of fetal formation, the cells do serve a purpose when they
are formed, but that purpose is only temporary. However, this is not unlike
many of your adult cells. The cells dying inside you right now probably had a
“job to do,” but now they are worn out and replacements have been made for
them. In essence, most of our cells are temporary.
Apoptosis is a group of complex mechanisms that allow cells to die
well. We all know about cells that do not die well. If you hit your thumb with
a hammer, you kill a few thousand cells. They tear open and dump their cellular
contents into the tissue around them. This signals a reaction called
inflammation and perhaps a sort of immune response. Inflammation and immune
responses are good at cleaning up the damage, but they can cause damage in the
process. With a million cells dying every second by apoptosis, you would never
survive if every death brought an inflammatory response.
Signals from outside the cell can stimulate apoptosis, including
hormones, damaging chemicals, or a loss of innervation. Sometimes it can be as
little as a cell migrating from where it should be; the lack of the proper
neighboring cells triggers the out of place cell to die. These are examples of extrinsic apoptosis.
But the signal could be intrinsic
as well. Signals that come from inside the cell could be DNA damage, too many
oxygen radicals causing damage to proteins, or even that the cell senses it has
been infected by a virus. Viruses turn the cell into a virus factory,
then the cell bursts to release the new viral particles and they go on to infect more
cells. By initiating programmed cell death, no new viruses are made, so no
additional cells will be infected and killed. As Spock would say, "They good of the many outweighs the good of the few, or the one."
The exceptional part about this process is that the mitochondrion is a crucial instigator in apoptosis. This organelle
that is so crucial for life and so important for giving the cell its energy to
carry out its functions, is one of the main checkpoints and instruments of programmed cell death.
If the signal for apoptosis comes from within the cell, it results
in a change in the membrane of the mitochondrion, with leakage of a protein
called cytochrome c out into the cytoplasm. Cytochrome c is usually held
within the mitochondrion, so that the apoptosis process is held in check. Once
released, this protein complexes with other proteins to form an apoptosome, and this starts a cascade
toward death.
If the signal comes from outside the cell, many different receptors
and pathways can be involved, but some of these will also affect the
mitochondria. There are competing sets of factors in the cytoplasm, some always
pushing toward cell death while others apoptosis from proceeding. The
delicate balance of the factors that want to disrupt the mitochondrion and
those that want to protect it allows the cell to live in harmony with itself
until there is a reason to die.
Apoptosis isn’t just for your looks, as in giving you individual
fingers and toes. It plays a role in every system of your body, in other
animals, and even in plants. Plant cells undergo a programmed cell death, but
it is a little different than animal apoptosis because they also have a cell
wall to deal with and they don’t have an immune system to ingest all the dying
cells. And the metamorphosis of caterpillars turning into butterflies and
tadpoles becoming frogs… that couldn’t happen without a lot of apoptosis.
Your embryonic and juvenile nervous system has millions of neurons
it does not need. The connections between some neurons may not be in accordance
with how humans process signals, and some dying back of processes and cells is
expected (called neural pruning).
Misplaced connections that do not die from apoptosis can lead to
some interesting results. Synaesthesia
is a group of conditions where sensory input is interpreted in more than one
area. For example, if connections between taste and other parts of the brain
are not pruned by apoptosis, some people will taste colors, or names will have
a certain taste. Many synaesthetes (people with synaesthesia) will see number
in their brains as having certain shape or texture. It is believed that most children
have near photographic memories and cross innervations among the senses, but
that the connections for these abilities die back in order to prevent sensory or
memory overload.
Your immune system also relies on apoptosis. You have T lymphocytes
that are designed to recognize a certain molecule that shouldn’t be in your
body. Each population of T cells recognizes a different potential problem guest
– millions of them in all. But some of the T cells that are made recognize a
particle that looks a lot like one of your own molecules. You don’t want that.
In your thymus and other places in your body, your T cells go
through a testing process. If they recognize a protein or molecule that isn’t
you, they are allowed to mature and then go out in to the body and patrol for
their particular target. But if they are programmed to recognize something that
is “self” then they are signaled to undergo apoptosis.
It is a great system and works most of the time, but there are
exceptions. Some “non-self” proteins can mimic “self” proteins, and if you
start to develop an immune response to them, there may be some cross-reaction
with your own cells. Or perhaps some T cells that recognize a “self” protein
don’t undergo apoptosis when they should. These issues can result in autoimmune
diseases – your immune system is attacking you.
Death is a part of life, and we should be thankful for it.
Novich, S., Cheng, S., & Eagleman, D. (2011). Is synaesthesia one condition or many? A large-scale analysis reveals subgroups Journal of Neuropsychology, 5 (2), 353-371 DOI: 10.1111/j.1748-6653.2011.02015.x
Hänggi, J., Beeli, G., Oechslin, M., & Jäncke, L. (2008). The multiple synaesthete E.S. — Neuroanatomical basis of interval-taste and tone-colour synaesthesia NeuroImage, 43 (2), 192-203 DOI: 10.1016/j.neuroimage.2008.07.018
Eroglu M, & Derry WB (2016). Your neighbours matter - non-autonomous control of apoptosis in development and disease. Cell death and differentiation PMID: 27177021
For
more information or classroom activities on apoptosis and synthaesthesia, see:
Apoptosis
–
Synaesthesia
–